For Providers
Are Nutrition Visits Covered?
Even without a nutrition-related diagnosis like diabetes, patients may have nutrition coverage under their preventive plan. Consider referring for a preventive diagnosis like Z71.3 (dietary counseling and surveillance). This might be useful for patients struggling with:
Chronic Dieting | Overeating | Emotional eating Orthorexia | Food preoccupation | Disordered eating | Body image concerns
Here are some more specifics for the insurance carriers Adina Pearson is contracted with:
Premera / Lifewise
Usually very good coverage. If not treating a specific medical diagnosis, nutrition counseling may fall under preventative health benefit which is typically covered in full by the plan. Diagnoses of either diabetes or eating disorders usually not subject to number of visit limits. Does not cover group nutrition classes (97804).
Regence / Uniform / Bridgespan / Asuris / HMA
Usually very good coverage. If not treating a specific medical diagnosis, nutrition counseling may fall under the preventative health benefit which is typically covered in full by the plan. Preventive visits and diagnoses of either diabetes or eating disorders usually not subject to number of visit limits (i.e. 3 per lifetime). Generally covers group nutrition classes (97804)
Kaiser Permanente of WA
HMO plans require a referral/prior authorization. They usually authorize 6 visits initially with re-authorization required for additional visits. Some have up to 24 visits/yr. PPO or "Options" plans do not require a referral or prior authorization to see an RD. Some plans have a different copay amount due for primary care visits vs. specialist visits. In most cases, KP considers RDs specialists. Generally covers group nutrition classes (97804)
First Choice Health / Moda
Physician referral typically not required.
Aetna
A medical referral and diagnosis is required. Please fax full diagnosis list, clinical notes and labs.
Diagnoses covered:
- Preventive "Healthy Diet Counseling" is covered at no cost for people with "obesity" alone, or "overweight" PLUS a cardiovascular risk factor (i.e. hypertension, dyslipidemia, impaired fasting glucose, or the metabolic syndrome).
- Most other diagnoses are covered as medical and may apply to deductible/copay.
- ADHD, asthma, and chronic fatigue are NOT covered.
- Aetna's policy on nutrition counseling
Cigna
We must receive medical diagnosis codes from a physician (or mental health provider for ED codes) in order to submit claims. At least 3 wellness/ preventative visits are covered per year in full by the plan. Additional visits are covered by most plans, though sometimes with a copay/coinsurance. Cigna's Preventative Care Services Policy
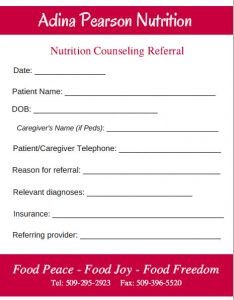
Referral Form
Thank you for referring your patients to nutrition counseling.
You can fax referrals to 509-396-5520
Click image below to use our adult or pediatric referral form.